Chiropractic Adjustment, known in scientific literature as Spinal Manipulative Therapy (SMT), is a specialized therapeutic approach performed by chiropractors. This method involves applying a controlled, rapid, low-amplitude force to the joints of the spine or other body joints.
The main objective is to restore or improve joint function, reduce pain, and optimize the overall performance of the musculoskeletal and nervous systems.
The philosophy of chiropractic is based on the principle that the body's structure, especially the spine, has a direct impact on neurological function and general health. This guide has been prepared adhering to the highest standards of scientific credibility
1. Decoding the Physiological Mechanisms: The Science Behind Manual Therapy
The effectiveness of chiropractic adjustments is not based solely on "popping bones back in place" but is rooted in complex neurological and mechanical reactions.
A) The "Pop" Sound (Joint Cavitation): Where Does It Come From?
One of the distinctive features of a chiropractic adjustment is the "pop" or "cracking" sound heard from the joint.
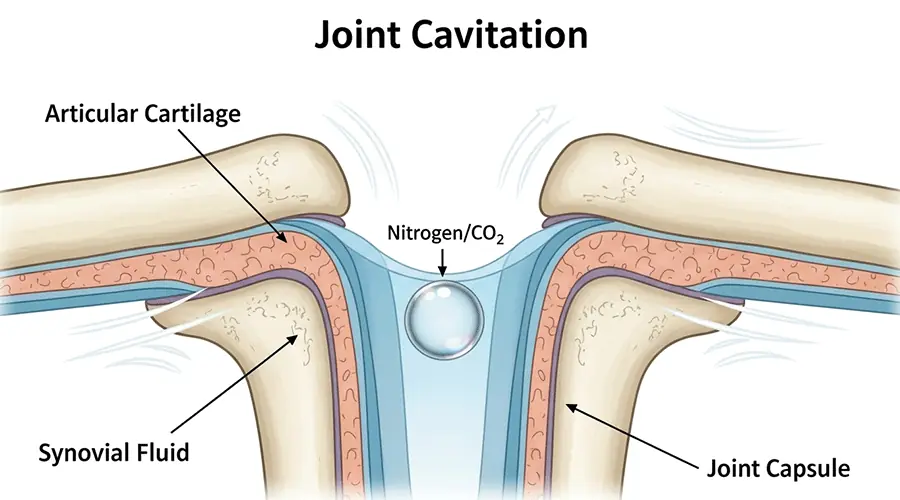
- Joint Cavitation: This phenomenon is the result of a process called Tribonucleation.
- Gas Bubble Formation: Our joints contain synovial fluid and dissolved gases (such as nitrogen, oxygen, and carbon dioxide). When a quick, controlled force is applied to the joint, the joint surfaces are rapidly separated, creating a sudden pressure drop within the joint capsule.
- Source of the Sound: As a result of this pressure drop, the dissolved gases rapidly change into a gas phase, forming a gas bubble or cavity. This rapid cavity formation creates the "pop" sound. This sound is in no way caused by bones breaking or colliding and is not the goal of the treatment itself, but a byproduct of the rapid joint movement.
B) The Nerve Reflex: The Key to Muscle Release
The most important therapeutic aspect of chiropractic adjustments is their impact on the nervous system and the muscles surrounding the spine:
- Activation of Neural Receptors: The rapid force applied activates specific nerve receptors called Golgi Tendon Organs (GTO). These receptors are sensitive to muscle stretch and tension.
- Autogenic Inhibition: GTO activation sends a neural signal to the spinal cord, which inhibits the Alpha Motor Neuron (the neuron commanding muscle contraction).
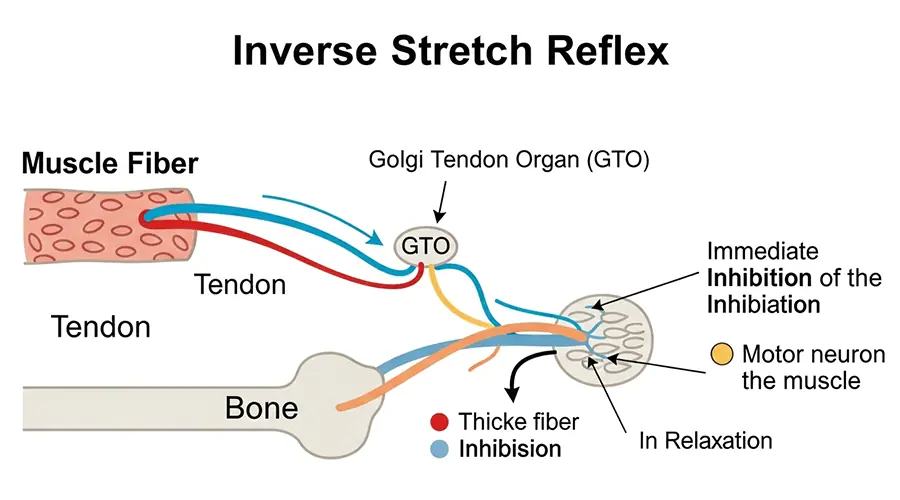
- Immediate Relaxation: This process, also known as the inverse stretch reflex, leads to a reflexive and immediate relaxation of the muscle that was in spasm or excessively contracted. This mechanism is purposefully used to break the pain-spasm-pain cycle.
C) The Concept of Subluxation: A Key Scientific Debate
- Traditional Definition: Some chiropractors define Vertebral Subluxation as a functional abnormality in the spine that can affect the nervous system, leading to a wide range of ailments beyond musculoskeletal issues.
- Modern Scientific View: Credible scientific evidence does not support the idea of "subluxation" as a cause of diseases unrelated to the musculoskeletal system. Many modern, evidence-based chiropractors consider this part of the theory lacking empirical support.
- More Accurate Term: In modern medicine, the more precise term "Segmental Joint Dysfunction" is used instead of "subluxation." This term specifically refers to restricted movement, localized pain, and muscle spasm in the spinal joints.
2. Evaluation and Treatment Process: From Diagnosis to Lasting Recovery
An effective treatment plan begins with accurate diagnosis and leads to lasting results through active patient participation.
A) First Session: Accurate Diagnosis

- Comprehensive History: Gathering a detailed medical history, including specific information on the nature of the pain, aggravating factors, and lifestyle habits (job, sleep, nutrition).
- Complete Physical Exam: Assessing posture, range of motion, palpation for painful areas, and specialized orthopedic and neurological tests.
- Diagnostic Imaging (X-ray/MRI): Prescribed only when "red flags" (such as a history of trauma, suspicion of infection, cancer, or disc herniation) are present.
- Individual Treatment Plan: Developing a personalized program including short-term goals (pain reduction) and long-term goals (full functional restoration and prevention of recurrence).
B) Treatment Sessions: Beyond a Simple Adjustment
- Typical Procedure: The patient usually lies on a special chiropractic table, and the practitioner performs the necessary adjustments using their hands or specialized instruments.
- Frequency and Duration: For an acute problem, 2 to 3 sessions per week for the first 2 to 4 weeks may be prescribed. As symptoms improve, the frequency decreases.
- Post-Treatment Sensation: It is entirely normal to feel mild soreness, aching, or fatigue for 24 to 48 hours after the session, similar to a reaction after exercise.
C) The Patient's Role: Active Participation for Lasting Results
- "Homework": Prescribing a set of stretching and strengthening exercises to stabilize treatment results achieved in the clinic.
- Education and Prevention: Educating the patient on posture correction (sitting, standing, and sleeping) and ergonomics in the workplace to help prevent the problem from returning.
3. The Chiropractor's Toolkit: Key Techniques and Their Applications
Chiropractors use a wide range of techniques. The choice of method depends on the patient's clinical status, age, comfort level, and the practitioner's expertise.
| Technique | Simple Description & Mechanism | Common Applications | Ideal Patient Profile |
|---|---|---|---|
| Diversified Technique | The most common method; uses a rapid, low-amplitude thrust (HVLA) to restore joint motion. Often accompanied by the "pop" sound. | Low back pain, neck pain, headaches. | Patients comfortable with higher-force manual treatment and no specific contraindications. |
| Activator Method | Uses a handheld, spring-loaded instrument to deliver a quick, low-force pulse to a specific point. No strong twisting or bending. | Seniors, children, patients with osteoporosis, or those who fear manual thrusts. | Seniors, children, patients with osteoporosis, or those who fear manual thrusts. |
| Thompson Drop Table Technique | Uses a specialized table with movable sections that "drop" slightly at the moment the thrust is applied. This assists gravity and requires less force. | Low back pain, neck pain, hip pain. | Patients requiring lower-force adjustments without excessive rotation. |
| Flexion-Distraction | Uses a moving table to apply rhythmic, gentle traction and bending to the lumbar spine. A very mild, non-thrust method. | Sciatica, disc herniation, spinal stenosis. | Patients with disc problems or severe sciatic pain. |
| Spinal Mobilization | Gentler, more stretching movements than the Diversified Technique. Involves moving the joint within its normal range of motion without a rapid thrust. | High-sensitivity patients, acute muscle spasms. | Patients in an acute phase of pain or those who cannot receive HVLA thrusts due to conditions like osteoporosis. |
4. Clinical Efficacy: Strong Evidence vs. Unsupported Claims
The efficacy of this treatment must be evaluated based on high-quality scientific evidence.
A) Conditions with Strong Evidence
- Acute and Chronic Low Back Pain: Has the strongest scientific support. SMT is recommended as an effective and first-line treatment option for acute, subacute, and chronic low back pain.
- Neck Pain: Substantial evidence supports the efficacy of SMT for managing mechanical neck pain. Results are optimized when manipulation is combined with exercise programs.
- Cervicogenic Headaches: Strong evidence shows that SMT can effectively reduce the frequency, intensity, and duration of these headaches, which originate from disorders in the upper neck joints.
B) Conditions with Moderate or Promising Evidence
- Sciatica (Radiculopathy): Moderate evidence suggests SMT, especially gentler techniques like Flexion-Distraction, is effective in reducing pain.
- Migraine and Tension Headaches: Some studies indicate SMT can act as an adjunctive treatment to reduce the frequency and severity of migraine attacks.
- Limb Joint Pain: Promising evidence exists for its use in conditions like shoulder pain, and mild-to-moderate arthritis of the knee and hip.
C) Unsupported Claims
To maintain transparency, the line between evidence-based applications and unsupported claims must be clearly drawn:
- Asthma: Comprehensive systematic reviews have failed to show any statistically significant improvement in objective pulmonary function. Chiropractic is not a primary treatment for asthma.
- Hypertension (High Blood Pressure): Research is extremely limited and contradictory. Currently, chiropractic is not considered an approved treatment for high blood pressure.
- Other Conditions: Claims regarding the treatment of non-musculoskeletal conditions like ear infections, digestive issues, allergies, or infertility lack credible scientific backing in modern medical literature.
5. Safety, Risks, and Contraindications: An Essential Risk Assessment
Chiropractic adjustments, when performed by a licensed, trained, and skilled professional, are generally considered a very safe therapeutic method.
A) Rare but Serious Complications: Analyzing Stroke Risk
- Most Serious Complication: The most serious rare complication associated with neck manipulation is stroke resulting from Cervical Artery Dissection (CAD).
- Statistics and Prevalence: The risk of this complication is extremely low (estimated at about 1 case per several million neck adjustments).
- Association vs. Causation: Evidence suggests that in many cases, the stroke is part of the progression of the underlying condition (artery dissection), not a direct result of the adjustment. Patients experiencing artery dissection often have initial symptoms like severe neck pain and headache, leading them to seek treatment.
- Importance of Screening: This highlights the critical importance of a thorough screening before any neck manipulation to identify warning signs.
B) Absolute and Relative Contraindications
In certain conditions, performing chiropractic adjustments may be dangerous and must be avoided:
| Absolute Contraindications (Prohibited) | Relative Contraindications (Requires Caution) |
|---|---|
| Severe Osteoporosis | Inflammatory joint diseases in the acute phase (e.g., Rheumatoid Arthritis) |
| Tumor or Cancer in the Spine | Use of blood-thinning medications (e.g., Warfarin) |
| Acute Fracture or Severe Instability in the spine | Severe spinal stenosis |
| Severe, progressive neurological symptoms (e.g., Cauda Equina Syndrome) | History of spinal surgery |
| - | Known vascular abnormalities in the neck arteries |
6. Chiropractic in the Healthcare Landscape: Comparison with Physical Therapy

While both disciplines focus on treating musculoskeletal disorders, they have key differences in philosophy and approach:
| Feature | Chiropractic | Physical Therapy |
|---|---|---|
| Core Philosophy | Focuses on manual joint adjustment and the nervous system to improve overall body function. | Focuses on improving movement, function, and quality of life through rehabilitation, exercise, and patient education. |
| Primary Intervention | Joint Adjustment/Manipulation as the main intervention to restore movement. | Prescribed exercise programs (strengthening, stretching), manual therapy (mobilization, soft tissue), and patient education. |
| When to Consult? | For acute or chronic spine pain (low back, neck) and related headaches that need joint movement restoration. | For comprehensive rehabilitation after injury or surgery, improving muscle weakness, and long-term management of chronic conditions through structured exercise. |
Conclusion
Chiropractic adjustments, when applied based on sound scientific principles and credible clinical evidence, are an effective, safe, and valuable therapeutic approach for managing a wide range of musculoskeletal and neurological disorders. The future of this field lies in further integration into mainstream healthcare, closer collaboration with other medical professionals, and focusing on its evidence-based strengths.
Frequently Asked Questions (FAQ)
Does a Chiropractic Adjustment Hurt?
No, you will not feel severe pain. The practitioner applies controlled pressure, which may be accompanied by the "pop" sound. The sensation after treatment is similar to mild soreness after exercise, which usually resolves quickly.
What Causes the "Pop" Sound During Chiropractic Adjustment?
The sound results from the formation of a gas bubble (cavitation) in the synovial fluid due to the sudden change in pressure when the joint surfaces are separated. The sound is not caused by bones hitting each other.
Is Chiropractic Good for a Herniated Disc or Sciatica?
Yes, there is strong evidence that chiropractic is effective for low back pain and moderate evidence for sciatica/disc herniation. Gentler techniques like Flexion-Distraction are often recommended for disc problems.
Is Chiropractic Dangerous?
No, chiropractic is generally very safe when performed by a licensed and trained professional. Serious complications (like stroke) are extremely rare, and thorough screening minimizes risk.



