Dry Needling has emerged as an effective and popular technique in physiotherapy for managing musculoskeletal pain. However, as with any medical intervention, patients often have questions about its potential side effects, especially in relation to chronic conditions like migraines. The central question for many is: Can dry needling cause migraines? This article will explore the answer.
What is Dry Needling?
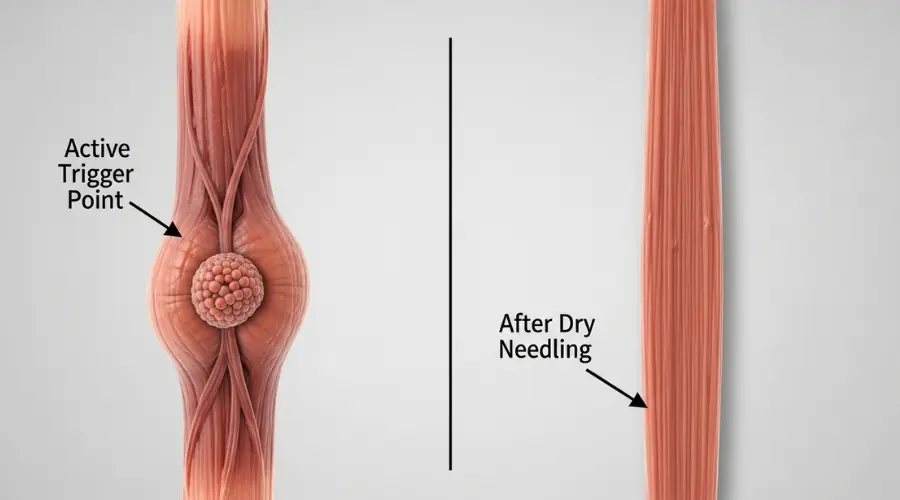
Dry needling is a technique performed by licensed physiotherapists and trained specialists. The method involves inserting a thin, sterile, solid needle (a "dry" needle because it contains no medication) into specific areas of the muscle known as Myofascial Trigger Points (MTrPs). Imagine a trigger point as a tight, highly irritable knot within a muscle that can cause pain not only at that spot but also in seemingly unrelated areas (referred pain). The goal of dry needling is to stimulate this trigger point, which results in a "Local Twitch Response" (LTR)—a brief, involuntary muscle contraction. This action is believed to help release muscle tension, improve blood flow, and break the pain cycle, ultimately leading to pain relief and improved muscle function.
The Connection Between Dry Needling and Migraines
Given that dry needling primarily targets muscle tension, especially in the neck and upper back—areas often implicated in tension headaches and the onset of some migraines—the relationship is complex. The prevailing view in specialized medical and physiotherapy communities is that dry needling is often used as a treatment for certain types of headaches, not a migraine trigger. Many tension-type headaches and even some migraines are linked to underlying muscular problems and active trigger points in the neck and shoulder muscles. By deactivating these trigger points, dry needling aims to reduce the frequency and intensity of headache attacks.
This complex relationship needs to be examined from two main aspects:
A) Targeted Treatment of Referred Pain
Many forms of chronic headaches, particularly Chronic Tension-Type Headaches (CTTH) and Cervicogenic Headaches (headaches originating from the neck), stem directly from active and latent MTrPs in the surrounding muscles.
- Key Muscles: The main muscles involved often include the Upper Trapezius, the small Suboccipital Muscles at the base of the skull, the Scalenes, and the Sternocleidomastoid (SCM) muscle.
- Mechanism of Relief: When the physiotherapist inserts the needle into the trigger point, a Local Twitch Response (LTR) is elicited. This response mechanically relaxes the shortened muscle fibers, initiates a healing process, and, crucially, dampens the referred pain signals to the head that are causing the headache. As treatment progresses, the patient's pain threshold increases, and the overall hyperexcitability of the Central Nervous System (central sensitization) is reduced. The net result is a significant decrease in headache attack severity and frequency.
B) Reducing Central Nervous System (CNS) Sensitization
The efficacy of needling in treating migraines that have a muscular tension component is rooted in its positive effect on the Trigemino-Cervical Complex (TCC).
The TCC Junction: The TCC is a crucial convergence area in the brainstem where sensory input from the face and head (via the Trigeminal nerve) meets sensory input from the neck and upper spine (via the upper Cervical nerves).
Role in Migraine: Active trigger points in the neck muscles constantly send pain signals to the TCC. In migraine-prone individuals, this continuous sensory input can lead to TCC hyperexcitability, thus making the Central Nervous System highly sensitized and increasing the likelihood of a full-blown migraine attack being triggered.
Needling Effect: By effectively deactivating these painful trigger points, the input flow of pain signals to the TCC is significantly reduced. This decrease in neural "noise" helps to calm the central nervous system, which, over time, may lead to a reduction in the overall frequency and intensity of migraine attacks.

Can Dry Needling Cause a Headache?
In rare cases, and typically as a mild and temporary side effect, some individuals report experiencing a headache after a dry needling session. This potential side effect is usually attributed to several factors:
- Post-Treatment Soreness: The targeted muscle groups, especially in the neck and upper back, may be sore, similar to muscle fatigue after a workout. This localized discomfort can occasionally present as a tension-type headache.
- Physiological Response: The treatment stimulates the nervous and vascular systems. In some sensitive individuals, this stimulation or the sudden release of muscle tension can temporarily result in a mild, transient headache.
- Dehydration or Stress: If the patient is dehydrated or highly anxious before or during the session, it can increase the likelihood of experiencing slight dizziness or a mild post-session headache.
It is crucial to distinguish between a mild, temporary post-treatment headache and a full-blown migraine attack. While a temporary headache may be experienced, supportive evidence for dry needling as a direct trigger for a severe clinical migraine, when performed correctly by a qualified professional, is generally not observed. In fact, many studies indicate the opposite—that dry needling can be an effective tool in a comprehensive migraine management program.
Precautions: Who Should Be Cautious?
While generally safe, dry needling is not appropriate for everyone, and certain individuals require careful assessment and discussion with their practitioner.
Patients who should exercise caution or fully discuss their condition include:
- Individuals with Chronic Migraines: Although dry needling may help, the patient's specific pain sensitivity and migraine triggers must be thoroughly assessed. The physiotherapist should start cautiously and monitor the patient's reaction closely.
- Individuals with Bleeding Disorders or on Blood Thinners: Due to the risk of excessive bleeding or bruising, patients with hemophilia or those taking anticoagulants require explicit clearance from their physician and careful consideration by the physiotherapist.
- Individuals with Severe Needle Phobia or High Pain Sensitivity: While the needles are very thin, the "twitch response" can be briefly uncomfortable. Patients with extreme anxiety or a low pain tolerance may find the procedure difficult.
- Patients with a Compromised Immune System or Active Infections: Any treatment involving skin penetration carries a minor risk of infection.

Practical Recommendations for a Safe and Effective Session
To get the best results and reduce any possible Side Effects of Dry Needling, you can take a few simple steps:
- Communicate Your Migraine History: Always inform your physiotherapist about the frequency, severity, and known triggers of your migraines. This information helps them customize the treatment, perhaps by starting with fewer points or shallower needling.
- Stay Hydrated: Ensure you drink plenty of water before and after the session. Dehydration is a common trigger for general headaches and post-treatment soreness.
- Use Calming Techniques: Arriving at the appointment in a relaxed state can be helpful. Techniques like slow, deep breathing during the procedure can reduce anxiety and muscle guarding.
- Listen to Your Body: If you feel unusual or excessive pain during the procedure, inform your therapist immediately. Rest immediately after the session and avoid strenuous activity.
Conclusion:
In summary, the best available evidence supports dry needling as a valuable tool for the comprehensive management of headaches. Far from being a primary cause, dry needling significantly helps to reduce the underlying muscular tension that contributes to pain. We have explored the question, can dry needling cause migraines?—and the consensus is that when performed correctly by a qualified practitioner, it is highly unlikely to trigger chronic migraines. Instead, it offers a non-pharmacological pathway to relieve musculoskeletal stress often associated with these conditions.
The safety and effectiveness of the treatment hinges on the expertise of the practitioner. Always ensure your dry needling is performed by a licensed, certified physiotherapist or qualified specialist. A professional possesses the deep understanding of anatomy, trigger point release, and safety protocols necessary to properly assess your unique situation, including your migraine history, and integrate dry needling into a holistic treatment plan that prioritizes your relief and long-term well-being.
Find out how dry needling can safely relieve your pain and tension. Visit our Dry Needling Service page to book a session with our experienced team.



