Back pain, a discomfort in the area between the lower edge of the ribs and the buttocks, is a common and widespread problem affecting approximately 80% of individuals at some point in their life, and it’s the leading cause of disability worldwide. This pain can range from mild discomfort to severe, debilitating agony, significantly impacting an individual’s quality of life. In this comprehensive article, we will explore the causes, symptoms, diagnostic methods, treatment options, and prevention strategies for back pain to help you better understand and manage this condition. Our aim is to provide comprehensive, reliable, and practical information that fully meets your needs and empowers you to take effective steps toward recovery and prevention of back pain.
What is Back Pain and What Are Its Types?
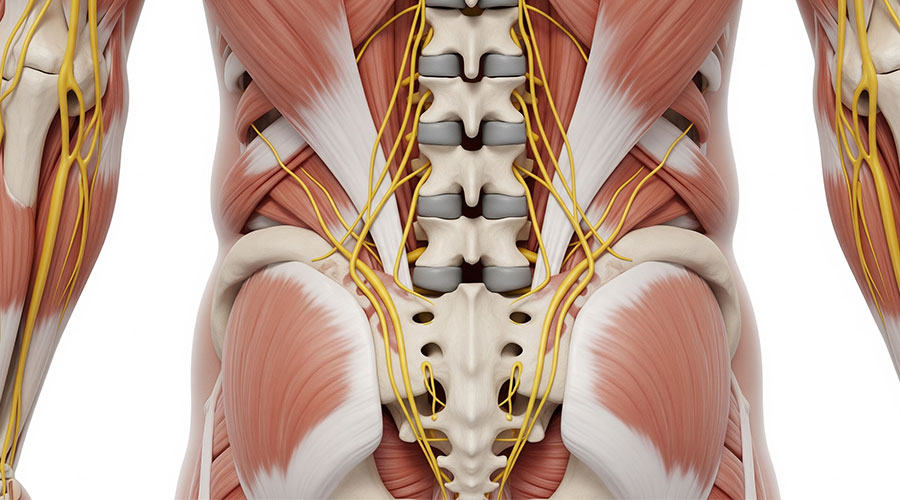
Back pain, also known as lumbago, refers to pain in the lower part of the lumbar spine, from below the ribs to above the buttocks. This pain can involve muscles, nerves, bones, discs, and other spinal structures.
Back pain can be classified based on its duration:
- Acute back pain: Pain that lasts less than 6 weeks. Most cases of acute back pain resolve on their own. “Symptoms of back pain typically improve within a few weeks from onset, with 40% to 90% of individuals recovering within six weeks.”
- Subacute back pain: Pain that continues for 6 to 12 weeks.
- Chronic back pain: Pain that persists for more than 12 weeks (three months).
Symptoms of Back Pain
Back pain symptoms can be highly varied and differ from person to person:
Pain: This pain can range from a dull, constant ache to a sharp, sudden sensation. It may be felt as throbbing, shooting, or burning.
Stiffness: It may become difficult to move or stand upright, especially after prolonged periods of inactivity.
Postural problems: Many individuals with back pain find it hard to stand straight or maintain proper posture, often due to pain or muscle spasms.
Muscle spasms: Uncontrolled and painful contractions of the back muscles, which can be very distressing.
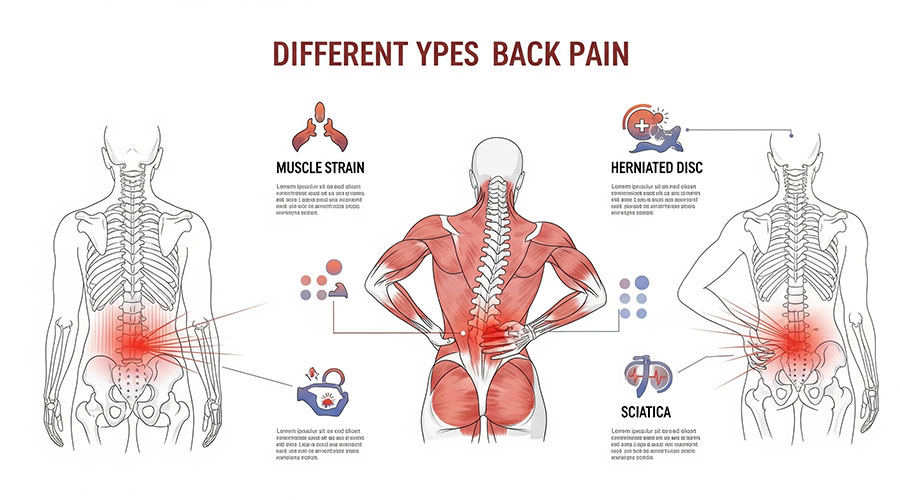
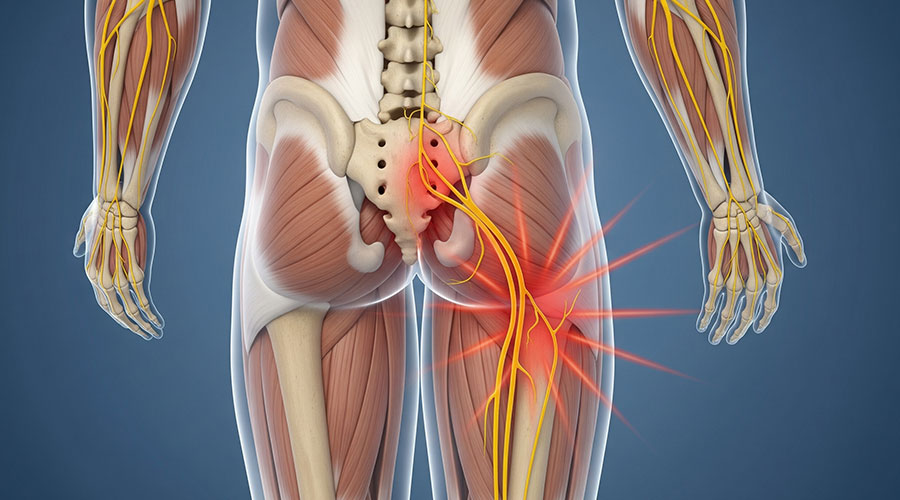
Radiating pain (Radiculopathy/Sciatica): Pain that extends into the buttocks or down the leg, often accompanied by numbness or tingling. This condition is frequently caused by pressure on the sciatic nerve and is known as sciatica.
Pain changes with position: Pain may worsen in specific positions such as bending over, prolonged sitting, coughing, or sneezing, and may improve with rest or lying down. For example, pain in spinal stenosis might improve with walking, while disc-related pain might worsen with prolonged sitting.
Causes and Risk Factors of Back Pain
Back pain can result from various reasons, but in most cases, its exact cause is not fully identified and is related to mechanical or musculoskeletal issues.
Most Common Causes of Back Pain
Muscle or ligament strain: The most common cause of back pain, often resulting from improper heavy lifting, sudden movements, excessive physical activity, or inappropriate exercise. This is typically benign and self-limiting
Disc problems:
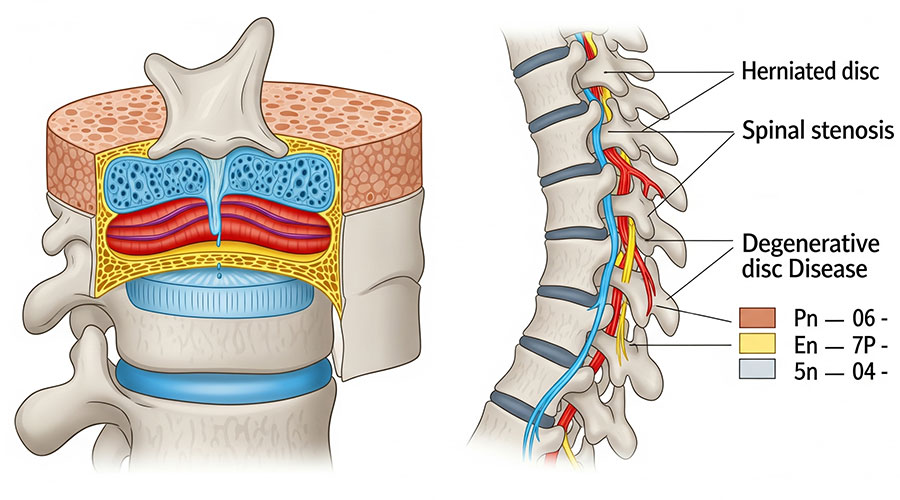
- Herniated or bulging disc: The spinal discs, located between the vertebrae, can bulge or rupture, putting pressure on nearby nerves.
- Degenerative disc disease: With age, discs may lose water, flatten, and lose their ability to absorb shock.
Structural spinal problems:
- Spinal Stenosis: Narrowing of the space around the spinal cord, which can compress nerves.
- Spondylolisthesis: A vertebra slipping out of place onto the one below it.
- Lumbar Scoliosis: An abnormal curvature of the spine to one side.
Arthritis:
- Osteoarthritis: Wear and tear of the spinal joints that can lead to pain and stiffness.
- Ankylosing Spondylitis: A type of inflammatory arthritis that affects the spine, causing stiffness and pain.
Other diseases and conditions:
- Tumors or infections: (Rarely) can cause back pain.
- Osteoporosis and compression fractures: Weakening of bones can lead to small, painful fractures in the vertebrae.
- Referred pain (Non-spinal): Pain originating from other organs like kidney stones, kidney infection, or abdominal aortic aneurysm that is felt as back pain.
- Fibromyalgia: A chronic condition causing widespread muscular pain, including back pain.
Many of these issues, such as disc problems and arthritis, are common throughout the entire spinal column and are also leading causes of Neck Pain.
Risk Factors for Back Pain
Age: The risk of developing back pain increases with age (typically after 30), as vertebral discs wear down over time.
Weight: “Individuals with a Body Mass Index (BMI) greater than 25 (overweight or obese) are at higher risk for back pain. Extra weight puts added stress on joints and discs.”
Physical activity: Both a sedentary lifestyle (lack of regular exercise) and excessive or improper physical activity can increase the risk of back pain.
Weak core strength: Weak abdominal and core muscles cannot adequately support the spine.
Smoking: Smoking can negatively impact blood flow to spinal discs and slow down the healing process. “Multiple studies have confirmed the link between smoking and back pain.”
Occupation and hobbies: Jobs requiring heavy lifting, frequent bending, or prolonged sitting increase the risk of back injury. Back pain is also very common in athletes.
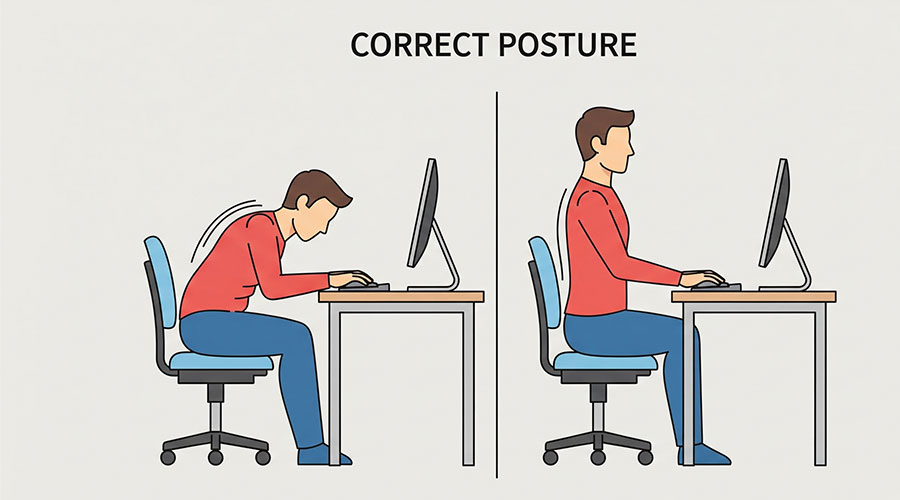
Poor posture: While sitting, standing, and sleeping can put extra strain on the spine.
Pregnancy: Hormonal changes and increased weight during pregnancy can lead to back pain.
Mental health: There is a link between depression, anxiety, and chronic back pain.
Weather: Some research suggests that changes in barometric pressure may affect joint pain, including back pain, however, strong scientific evidence directly linking weather to back pain is lacking, and further research is needed.
When to See a Doctor?
While most back pain resolves on its own, certain warning signs (red flags) indicate a more serious underlying problem and require immediate medical attention or emergency care.
Immediate Symptoms
- Severe pain after a serious accident or significant trauma (e.g., fall from height).
- Pain, numbness, weakness, or tingling in both legs.
- Numbness or tingling around the genital or buttock area (saddle anesthesia).
- Difficulty urinating or loss of bladder/bowel control (Cauda Equina Syndrome – a medical emergency).
- Chest pain accompanied by back pain.
- High fever and chills accompanied by back pain.
Symptoms Requiring Early Doctor Visit:
- Pain that persists for more than 72 hours or several weeks, or worsens.
- Unexplained and unintentional weight loss.
- History of cancer.
- Severe pain at night or at rest that does not improve with position changes.
- Age over 55 and onset of back pain without a clear reason.
- Weakened immune system (e.g., due to immunosuppressants or specific diseases).
- Chronic corticosteroid use.
- Severe pain after back surgery in the past year (risk of infection).
Important Note: “Performing diagnostic imaging or laboratory tests within the first four weeks after symptom onset has not been shown to be beneficial.” Routine imaging in the absence of warning signs is often unnecessary and can lead to unwarranted costs. It can also lead to incidental findings that are not necessarily related to the patient’s pain, causing unnecessary concern or unwarranted interventions.
Once you decide to seek professional help, preparing for your appointment by knowing the key questions to ask can make your treatment far more effective.
Diagnosing Back Pain
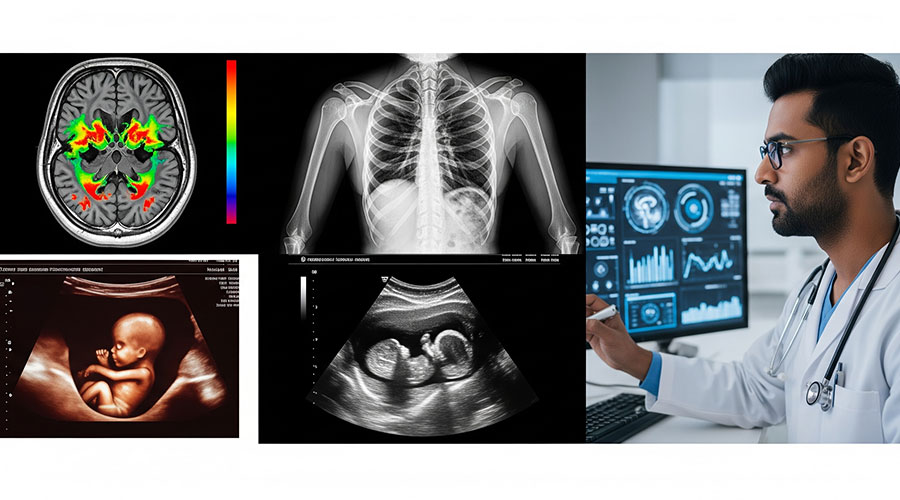
Diagnosing back pain often begins with a thorough clinical examination and a detailed medical history from the patient. The doctor will ask about the type of pain, its onset, aggravating and alleviating factors, and your medical history.
Physical examination: The doctor will palpate your spine, check your range of motion, and may perform specific tests like the Straight Leg Raise Test to check for disc herniation or nerve compression. This examination also assesses muscle strength, reflexes, and sensation.
Imaging:
- X-ray: Can reveal bone problems such as fractures, arthritis, or structural abnormalities.
- MRI or CT scan: These methods provide more detailed images of soft tissues such as discs, nerves, the spinal cord, and muscles, and are useful for diagnosing disc herniation, spinal stenosis, or tumors. However, MRI or CT scans are often not needed in the early stages unless red flags are present.
Laboratory tests: Blood or urine tests may be recommended to check for specific causes such as inflammation, infection, or kidney stones.
Electromyography (EMG): This test measures the electrical activity of muscles and can diagnose nerve damage.
Back Pain Treatment and Management Options
Back pain treatment depends on the underlying cause, severity, and duration of the pain. The approach is often conservative and involves a combination of methods.
Initial Approach and Home Care:
- Brief rest: Complete and prolonged bed rest is not recommended. “It is not recommended for more than 1-2 days,” followed by a gradual return to normal activities within pain tolerance. Continuing normal activities within pain tolerance is much better than absolute bed rest and accelerates recovery.
- Cold and hot compresses: Using cold compresses (ice) during the first 24 to 48 hours to reduce inflammation, and then hot compresses to relax muscles and increase blood flow, can be helpful.
- Over-the-counter (OTC) medications: Acetaminophen (paracetamol), ibuprofen, or naproxen (NSAIDs) are often effective for mild to moderate pain.
- If your back pain has just started, the best approach is to make a note of it and continue your normal activities.
Chiropractic, Physiotherapy, Physical Therapy and Therapeutic Corrective Exercise:
Effective, Non-Surgical Treatment for Your Back Pain
Two of the most effective conservative treatments to resolve back pain are Physiotherapy and Chiropractic care. These therapies target the root cause of your pain to provide lasting relief without medication or surgery.
Learn more about how our expert team can help you.
- Importance: “Physical Therapy (PT) can strengthen your muscles to better support your spine. PT also improves flexibility and helps you prevent another injury.” The importance of regular follow-up with a physical therapist for correct exercise instruction and individualized treatment plan development is crucial.
- Chiropractic spinal adjustments, mobilizations, and manual therapy could benefit most patients.
- Types of exercise:
Aerobic exercises: Such as walking, swimming, or cycling, help improve blood flow and reduce pain.
Core strengthening exercises: Strengthening abdominal and back muscles for better spinal support. Examples of beneficial exercises include bridges, bird-dogs, and planks.
Stretching exercises: Stretching tight muscles in the back, hips, and legs can improve flexibility. Examples include spinal twists, piriformis stretches, and child’s pose.
Yoga and Pilates: Especially for chronic pain, they can help strengthen muscles, improve flexibility, and posture.
Practical advice: It is recommended to watch instructional videos for proper exercise execution to avoid improper form. “These exercises can relieve your pain in 60 seconds.”
Manual Therapies:
- Chiropractic and spinal adjustments, mobilizations, and manual therapies: Therapists use manual techniques to adjust the spine and reduce pressure on nerves.
- Manual therapy: Can help relax tight muscles, reduce spasms, and improve circulation.
Prescription Medications:
- Prescription NSAIDs: If OTC medications are ineffective.
- Muscle relaxants: For severe and short-term spasms.
- Opioids: “Clearly explaining the high risks of addiction and side effects, and advising against their use as a first-line treatment.” The use of these medications should be under strict medical supervision and only for severe, short-term pain.
- Antidepressants and anticonvulsants: May be prescribed in specific cases of chronic back pain (e.g., neuropathic pain), but their role is limited or proven ineffective in many cases.
Advanced Therapeutic Modalities
Dry Needling: For targeting deep muscular trigger points and spasms that contribute to back pain.Dry Cupping: To improve local blood flow and release tension in the back muscles
Injections:
- Epidural steroid injections: Injecting corticosteroids into the epidural space (around the spinal cord) to reduce inflammation and pain. “May be recommended for managing chronic back pain, but they often offer no long-term benefit and can have side effects.”
- Nerve block: Injecting anesthetic agents around specific nerves to relieve pain.
Surgery:
When?: Surgery for back pain is “rarely necessary” and “only about one in ten patients needs back surgery.” This option is only considered in very specific and severe cases that do not respond to other treatments, or in emergency situations (like cauda equina syndrome), such as:
- Disc herniation with severe neurological symptoms (significant leg weakness, bladder problems, or loss of bowel control).
- Severe spinal stenosis causing disability.
- Severe structural abnormalities.
- Types of surgery: Discectomy (removing part of the disc), spinal fusion (merging vertebrae).
Psychological and Educational Approaches:
- Cognitive Behavioral Therapy (CBT): This type of therapy helps individuals cope with chronic pain, change negative beliefs about pain, and develop healthier coping skills.
- Patient education: Understanding the condition, the cause of pain, and self-management strategies is very important.
Preventing Back Pain

Prevention is always better than cure. By following these tips, you can minimize the risk of developing back pain:
- Maintain a healthy weight: Reduces pressure on the spine and discs. “Individuals with a Body Mass Index (BMI) greater than 25 (overweight or obese) are at higher risk for back pain.”
- Strengthen core and back muscles: Through regular exercise, especially core exercises (such as Pilates and yoga).
- Lift objects correctly: Always bend from your knees, keep objects close to your body, and avoid sudden twisting of the torso when lifting heavy objects.
- Maintain proper posture: While sitting, standing, and sleeping. Use ergonomic chairs and ensure your workstation is properly adjusted to support the natural curve of your lower back, monitor at eye level, and use a footrest if needed. Also, remember to change positions and take short breaks during prolonged work.
- Stay active: Regular exercise and daily physical activity help maintain spinal health, including walking and swimming.
- Quit smoking: Smoking compromises disc health.
- Ergonomic adjustment of the workplace: Ensure your desk, chair, and monitor are set up to maintain proper posture.
Outlook and Prognosis
- Acute pain: Often improves within a few weeks (40-90% in 6 weeks).
- Recurrence: Unfortunately, more than half of individuals may experience pain recurrence.
- Chronic pain: Can be persistent, but treatments and management strategies can help reduce pain and improve quality of life.
- Factors influencing prognosis: Mental health, coping skills, fear of activity, and an individual’s expectations for recovery can all impact the final outcome.
